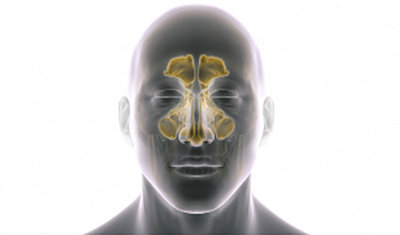
Sinusitis
Affects 31 million adults across the U.S.¹
Chronic sinusitis is an inflammation or swelling of the sinus lining and drainage pathways, which can lead to blocked sinuses. It can be brought on by several different issues and can be difficult to treat. Symptoms tend to persist and reoccur frequently despite the use of medicine. Sinusitis can affect both adults and children and the condition can have a negative impact on their lives.²
CAUSES
Chronic sinusitis can be caused by a variety of reasons including:2
- infection
- allergens
- bacteria
- inflammation of the nasal lining
SYMPTOMS
Sinusitis can be characterized by numerous symptoms. It is important to consult with your doctor to help determine the diagnosis and the best course of treatment. Symptoms include:3
- Facial pressure and pain
- Fatigue
- Low fever
- Frequent stuffy nose
- Nasal blockage
- Reduced sense of taste and smell
- Congestion or stuffy nose
- Headaches

TREATMENT
There are a range of treatment options for sinusitis patients to explore with your doctor, ranging from over the counter medications to surgical procedures.5
- Medication therapy: To help alleviate sinusitis symptoms, a primary care doctor may recommend prescription or over-the-counter medications, and/or home remedies.5
- Balloon sinus dilation: Balloon sinus dilation is a procedure that gently expands the natural sinus openings to fix underlying drainage problems.6
- Sinus surgery: Functional endoscopic sinus surgery (FESS) is appropriate for some chronic sinusitis sufferers. This procedure aims to improve sinus drainage by clearing the common drainage pathways to allow for normal flow of mucus. This is most often achieved by removing nasal structures and expanding the natural openings of the sinuses.7 Balloon sinus dilation can also be used in a FESS procedure to help open the natural drainage pathways from the sinuses.8
Balloon dilation treatment option:
What is balloon sinus dilation?
Balloon sinus dilation is a procedure performed to expand the blocked sinus drainage pathways.6 The device is designed to reshape your sinus pathways by inflating a small balloon in key anatomic locations, allowing for restored sinus drainage.8 This technique allows for the opening of the sinuses while preserving tissue and important nasal structures.9
Balloon sinus dilation:
- Is minimally invasive9
- Can be performed at the office, ambulatory surgery center (ASC) or hospital
- Can provide long-lasting relief10
WHAT TO EXPECT WITH TREATMENT
First, your doctor will numb the inside of your nose to ensure comfort during the procedure. Next, the doctor will place a small balloon in the opening of the targeted sinus. The balloon is gently inflated, expanding the opening and restoring the sinus drainage pathway. The balloon is then deflated and removed. Your doctor will continue to treat your other sinuses as needed.8
What to expect after treatment?11
Your doctor may instruct you to:
- Avoid blowing your nose for 24-48 hours
- Use a nasal saline to rinse your nose
- Sleep with your head elevated
- Avoid strenuous activity 1 week post procedure
- Always follow the instructions of your physician
For important safety and risk information, visit important risk and safety information for patients.
FAQ
Chronic sinusitis is an inflammation or swelling of the sinus lining and drainage pathways, which can lead to poor or blocked sinus drainage. It can be brought on by a number of different issues and can often be difficult to treat, with symptoms persisting despite treatment or recurring frequently.2
Although these conditions have similar symptoms, acute sinusitis only temporarily affects a person, while chronic sinusitis can last for 12 weeks or more. With chronic sinusitis, the severity of symptoms may change but will not completely resolve. Acute sinusitis symptoms resolve in four weeks or less. Recurrent sinusitis is classified as four or more acute sinusitis outbreaks in a single calendar year. Periods of relief are followed by another breakout.3
Balloon sinus dilation has been shown to be both safe and effective for children with chronic rhinitis 2 years and older.11*
*The XprESS ENT dilation system is indicated for use in the maxillary ostia/ethmoid infundibula in patients 2 years and older, and frontal ostia/recesses and sphenoid sinus ostia in patients 12 years and older.
Most patients can expect long lasting relief after a balloon sinus dilation procedure. Studies have demonstrated positive impact on patient lives by reduction of:10
- Missed work and school days
- Doctor visits
- Infections
- Antibiotic prescriptions
Most balloon sinus dilation patients resume normal activity in one to two days.10
Possible adverse effects include, but are not limited to, the following:8
- Pain
- Tissue inflammation
- Bleeding
- Cerebrospinal fluid leak
- Continued or worsening symptoms
- Orbital complications
Refer to the important risk and safety information link and speak with your doctor for a complete listing of potential side effects and risks.
Related products

XprESS® ENT dilation system
The XprESS ENT dilation system delivers control and versatility for balloon dilation. Its seeker-based design and tip malleability provides tactile feel and flexibility to address complex anatomy for a broad range of patients.8,12
References
- Bleier, Benjamin S., and Marianella Paz-Lansberg. "Acute and Chronic Sinusitis." Medical Clinics 105.5 (2021): 859-870.
- Battisti AS, Modi P, Pangia J. Sinusitis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470383/
- Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2S):S1–S39.
- Kaliner M. Medical management of sinusitis. Am J Med Sci. 1998 Jul;316(1):21-8. doi: 10.1097/00000441-199807000-00004. PMID: 9671040.
- Mayo Clinic. “Chronic Sinusitis.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 16 July 2021, https://www.mayoclinic.org/diseases-conditions/chronic-sinusitis/diagnosis-treatment/drc-20351667.
- Piccirillo JF, Payne SC, Rosenfeld RM, et al. Clinical Consensus Statement: Balloon Dilation of the Sinuses. Otolaryngology–Head and Neck Surgery. 2018;158(2):203-214. doi:10.1177/0194599817750086
- Hao Z, Gu H, Li W. The Efficacy of Functional Endoscopic Sinus Surgery Combined With Triamcinolone Acetonide Aqueous Nasal Spray for the Treatment of Chronic Rhinosinusitis. Front Surg. 2022 May 27;9:855618. doi: 10.3389/fsurg.2022.855618. PMID: 35711705; PMCID: PMC9197098.
- XprESS instructions for use 4322-001
- Lofgren DH, Shermetaro C. Balloon Sinuplasty. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546671/
- Chandra RK, Kern RC, Cutler JL, Welch KC, Russell PT. REMODEL larger cohort with long-term outcomes and meta-analysis of standalone balloon dilation studies. Laryngoscope. 2016 Jan;126(1):44-50. doi: 10.1002/lary.25507. Epub 2015 Jul 30. PMID: 26228589; PMCID: PMC5132108.
- Soler ZM, Rosenbloom JS, Skarada D, Gutman M, Hoy MJ, Nguyen SA. Prospective, multicenter evaluation of balloon sinus dilation for treatment of pediatric chronic rhinosinusitis. Int Forum Allergy Rhinol. 2017;7(3):221-229.
- Data on file at Stryker DHF 1656-001
The information presented is for educational purposes only. Stryker is not dispensing medical advice. Please speak to your doctor to decide what course of treatment is right for you. Only your doctor can make the medical judgment regarding which products and treatment is right for you. Any medical procedure carries certain risks and your doctor will explain all possible complications and/or side effects. The lifetime of any treatment is not guaranteed and varies by individual and each patient will experience a different post-operative activity and comfort level.
ENT-XPR-SYK-624152
